Exploring the nuances of telehealth vs telemedicine is essential for understanding modern healthcare delivery. As digital health continues to evolve, distinguishing these terms becomes crucial for patients seeking remote care and professionals providing it. This article addresses the key differences, uses, and examples of telehealth and telemedicine, offering clear insights for an informed approach to digital healthcare.
What is the definition of telehealth?
Telehealth is the utilization of digital and telecommunication technologies to provide and enhance healthcare services, education, and health administration from a distance. It encompasses a broad range of applications, not only facilitating clinical patient care through remote interactions but also extending to non-clinical services such as healthcare provider training, administrative meetings, and continuous medical education.
This approach integrates various technologies like video conferencing, the internet, and wireless communications to support healthcare delivery, public health, and health administration, enabling professionals like nurses, pharmacists, and social workers to offer educational, social support, and medication management services. By bridging geographical distances, telehealth improves access to healthcare services, making it an essential component of modern healthcare systems.
What are the benefits of telehealth?
The advantages of telehealth can be effectively categorized into benefits for patients and healthcare professionals, each enhancing the healthcare experience from different perspectives.
For patients:
1. Enhanced health monitoring: Telehealth introduces an innovative approach to health monitoring, allowing for timely preventive measures through remote technology. Devices that track vital signs like weight, blood pressure, and heart rate can relay data directly to healthcare providers, facilitating early detection of health issues.
2. Mobile health accessibility: Through mobile health platforms, individuals can receive ongoing health updates and educational resources on their mobile devices. This method supports continuous patient engagement and healthcare delivery, irrespective of physical location.
3. Streamlined video consultations: Live video consultations provide a direct channel for patients to discuss their health concerns, treatment plans, and laboratory results with their doctors, enhancing the quality of care and collaboration across geographic boundaries.
4. Cost reduction: Telehealth can significantly lower the costs associated with healthcare by minimizing the need for physical infrastructure and maintenance, thereby making high-quality healthcare more accessible and affordable.
5. Improved rural access: Virtual healthcare technology makes specialist care accessible to patients in rural areas, overcoming traditional barriers such as distance, transportation, and limited mobility.
6. Convenience and flexibility: The ability to consult with healthcare providers from home offers unparalleled convenience, reducing the need for time off work, travel expenses, and the stress associated with in-person visits.
For healthcare providers:
1. Flexible scheduling: Telehealth facilitates a more flexible schedule, allowing providers to intersperse telehealth sessions with in-person visits, enhancing productivity and care delivery.
2. After-hours service provision: The integration of secure telehealth systems enables providers to offer services outside traditional hours, increasing revenue opportunities without the necessity of being physically present in an office.
3. Lower absence rates: The convenience of telehealth appointments leads to fewer cancellations and no-shows, ensuring a more efficient and reliable schedule for healthcare providers.
4. Seamless follow-up process: Telehealth simplifies the process of scheduling follow-up visits and enables providers to easily conduct check-ins with patients, which is crucial for discussing test results, managing chronic conditions, and ensuring medication compliance.
5. Home-based care for chronic and post-acute conditions: Telehealth is instrumental in the management of chronic diseases, post-hospitalization care, and medication adherence, allowing providers to deliver care to patients in their homes, which supports the broader goals of value-based care systems.
What is telemedicine?
Telemedicine is the practice of delivering medical services and care remotely through telecommunications technology, enabling healthcare providers to diagnose, treat, and manage patients' health without requiring physical presence. It utilizes tools like phones, video conferencing, and other digital communication devices to connect medical professionals with patients across distances.
This approach is particularly valuable for individuals in remote, rural, or underserved areas where access to healthcare services is limited. Telemedicine offers a range of services, including but not limited to prescription management, chronic condition oversight, follow-up consultations, and access to specialist care, all facilitated over secure connections.
What are the benefits of telemedicine?
The benefits of telemedicine can be encapsulated into several key points, reflecting advantages for both patients and healthcare providers while incorporating a holistic view of healthcare delivery improvements.
For patients:
1. Lower infection risk: The absence of physical contact significantly reduces the chance of transmitting infections between healthcare professionals and patients.
2. Access around-the-clock: Medical attention becomes immediately available regardless of time, ensuring that patients receive care during emergencies or at times that would otherwise be inconvenient.
3. Support for chronic conditions: Ongoing management and monitoring of chronic diseases are facilitated, allowing patients to maintain their health without the need for frequent hospital visits.
4. Mental health care: Accessible psychiatric care provides personalization and promotes quicker recovery through remote sessions, enhancing the mental well-being of patients.
5. Extended healthcare access: Patients, especially those in rural or underserved regions, can consult with specialists and receive treatments previously unavailable to them, bridging the gap in healthcare accessibility.
6. Convenience and reduced costs: Patients save time and money by eliminating the need to travel, reducing wait times, and minimizing ancillary expenses such as childcare or time off from work.
7. Family involvement: The ability for family members to participate in the care process, even when not physically present, fosters a supportive environment and enhances patient care.
For healthcare providers:
1. Wider patient reach: A broader reach is possible through telemedicine, attracting more patients due to its convenience and efficiency, effectively filling providers' schedules.
2. Enhanced collaboration: Seamless communication among healthcare teams, including specialists, leads to better patient outcomes and faster decision-making in treatment processes.
3. Increased patient compliance: The likelihood of patients adhering to treatments and medications improves with easier access to care and more frequent communication.
4. Streamlined follow-up: Monitoring patients' progress and adjusting treatments as necessary becomes simpler through digital platforms, enhancing patient care and engagement.
5. Optimized health outcomes: A proactive approach to managing patient health reduces hospital readmissions and improves the management of both chronic and acute conditions from a distance.
6. Provider well-being: A better work-life balance is promoted for healthcare workers by mitigating the stress associated with in-person visits and providing more flexible scheduling options.
7. Operational cost savings: Overhead costs related to the physical delivery of care, such as facility maintenance and staffing, are decreased, making the healthcare delivery process more efficient.
Empower your healthcare strategy—download your free guide "From Leadership to Practice: Enhancing Modern Healthcare through Strategic Integration" today!
What are the key differences of telehealth vs telemedicine?
The key distinctions between telehealth and telemedicine lie in their scope and the range of services they encompass within the healthcare system. Although both utilize technology to enhance healthcare delivery, they serve different functions and cover various aspects of patient care and healthcare management.
Telehealth:
- Broad spectrum: Telehealth represents a wide-ranging use of technology in healthcare, covering both clinical and non-clinical services. This broad term includes everything from remote monitoring and healthcare provider training to administrative meetings and continuing medical education.
- Diverse participants: It involves a variety of healthcare workers, including healthcare professionals, educators, pharmacists, and frontline workers, all contributing to the delivery and support of healthcare services.
- Comprehensive services: Telehealth extends to a vast array of services beyond direct patient care, such as lab test reports, healthcare education, technology-healthcare sector collaboration, and support for chronic disease management through tracking and communication tools.
Telemedicine:
- Clinical focus: Telemedicine is specifically concerned with remote clinical services, facilitating the exchange of medical information between healthcare providers and patients for diagnosis, treatment, and monitoring purposes.
- Direct patient care: The core of telemedicine is the physician-patient interaction, primarily involving healthcare providers in the delivery of medical services through digital platforms.
- Limited scope: Compared to telehealth, telemedicine has a narrower focus, centering on the digital delivery of healthcare services by physicians, which includes consultations, follow-up visits, and the management of various health conditions.
Telehealth vs telemedicine examples
Telehealth examples:
Telehealth encompasses a wide array of services and applications that extend beyond direct patient care, illustrating the versatility and breadth of technology in healthcare. These examples include both clinical and non-clinical services:
1. Secure communication: Healthcare providers can send patient examination notes, medical histories, and radiographic images to specialists using secure email systems, enhancing collaborative care and specialist consultations.
2. Continuing education: Healthcare professionals have the opportunity to attend online lectures or complete courses for continuing medical education, keeping up to date with the latest advancements in their field.
3. Care coordination meetings: Teams of healthcare professionals can utilize video conferencing platforms to discuss and coordinate the care of patients, ensuring a unified approach to patient treatment plans.
4. Health tracking and information apps: Mobile and web applications that allow users to monitor their health statistics, such as blood pressure or cholesterol levels, and access general health information or alerts about disease outbreaks in their area.
Telemedicine examples:
Telemedicine, a subset of telehealth, specifically refers to the remote delivery of clinical services. Here are several examples that showcase the range of telemedicine services:
1. Virtual consultations: Remote video conferences enable physicians to diagnose, treat, and prevent diseases by interacting with patients in real time, regardless of their physical locations.
2. Medication management: Annual wellness visits, medication prescriptions, and refills can be handled online, along with specific consultations like nutrition or mental health counseling.
3. Specialized care: Urgent care for conditions such as rashes, sinus infections, and other non-emergency issues can be addressed through telemedicine platforms, along with remote monitoring of vital signs for ongoing health issues.
4. Post-operative care: Follow-up visits conducted via text, phone, or video conferencing allow for efficient post-operative monitoring and vital signs transmission, aiding in the management of recovery and chronic conditions.
When to use telemedicine and telehealth
Deciding between telehealth and telemedicine depends on the nature of the medical services required and the specific circumstances of the patient. Telemedicine, focusing on the delivery of clinical services remotely, is typically utilized when seeking medical care that doesn't necessitate an in-person visit. Here are guidelines on when to use each:
When to use telemedicine
1. Minor illnesses and conditions: Telemedicine is ideal for managing conditions like colds, flu, allergies, bronchitis, conjunctivitis, skin rashes, respiratory infections, sore throats, and minor infections.
2. Managing chronic conditions: Patients with ongoing health issues can benefit from regular telemedicine visits for monitoring and management without the need to travel.
3. Mental health support: It's particularly useful for therapy sessions, psychiatric evaluations, and ongoing mental health counseling.
4. Medication management: For prescription refills or discussing medication adjustments, telemedicine offers a direct line to healthcare providers.
5. Specialist consultations: Specialists, including surgeons for post-operative care, gynecologists for birth control consultations, and endocrinologists for lab result discussions, can provide their services remotely.
6. COVID-19 Screenings: Telemedicine has been instrumental in providing initial screenings and advice for COVID-19, reducing the risk of spreading the virus.
When not to use telemedicine
Severe symptoms: In cases of severe symptoms, such as shortness of breath, chest pain, or serious injuries, in-person emergency care is crucial.
When to use telehealth
Telehealth, encompassing a broader range of services beyond clinical care, is beneficial in several non-clinical contexts:
1. Education and training: Healthcare professionals can use telehealth platforms for continuing education, attending webinars, and participating in training sessions.
2. Care coordination: A team of healthcare professionals may utilize telehealth to discuss and coordinate a patient's care, especially in complex cases requiring multi-disciplinary input.
3. Remote monitoring: Patients with mobility issues or those living far from healthcare facilities can have their health monitored through devices that transmit data to their healthcare team.
4. Public health alerts: Telehealth services can disseminate important public health information, including disease outbreak notifications and health education materials.
How adam.ai streamlines the process of telehealth and telemedicine
As we've explored the distinctions and synergies between telehealth and telemedicine, it's evident that effective digital tools are essential for streamlining these services. One such solution is adam.ai, a comprehensive board management software platform. Equipped with video conferencing, action tracking, content management, analytics dashboard, meeting minutes features, and more, adam.ai facilitates the seamless operation of telehealth and telemedicine meetings.
Here's what you can do with adam.ai:
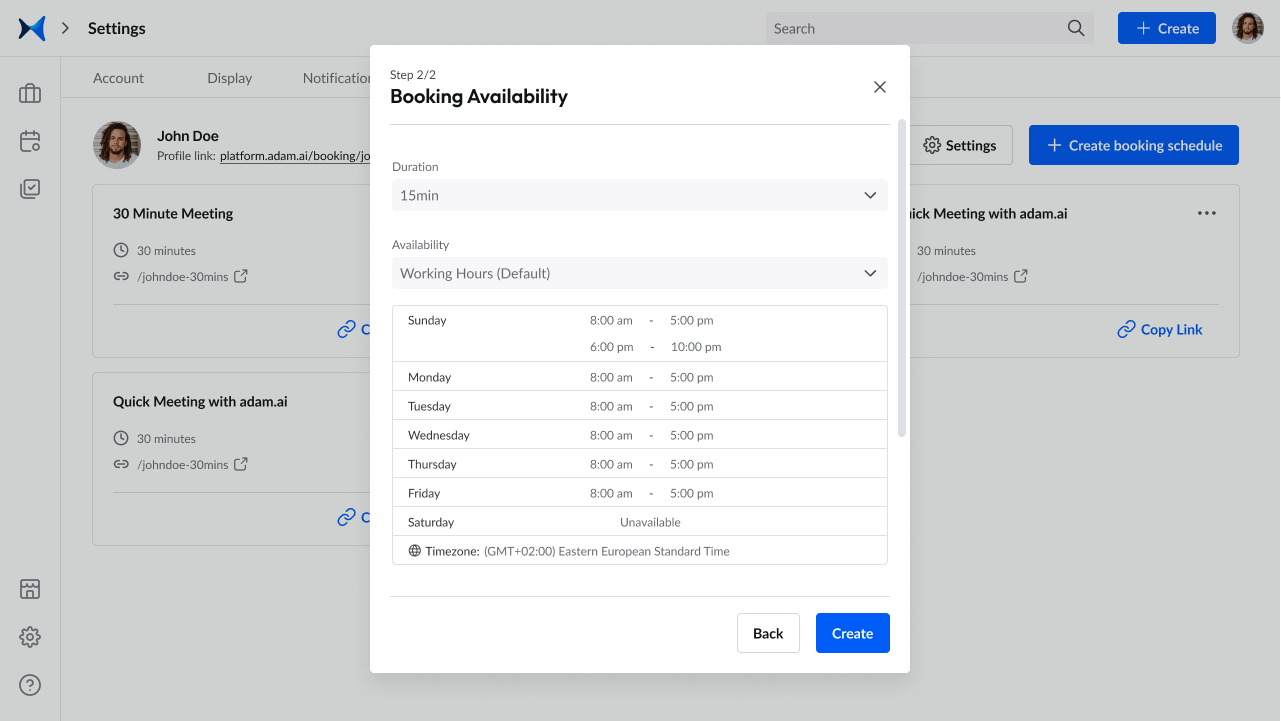
1. Simplified scheduling for meetings across the diverse network of healthcare professionals, ensuring critical collaboration between specialists, primary care providers, and other stakeholders without the logistical challenges of in-person meetings.
2. Integrated smart note-taking and video conferencing to facilitate real-time discussions on patient care plans, making it easier to share updates, deliberate on treatment options, and reach consensus with immediacy and clarity.
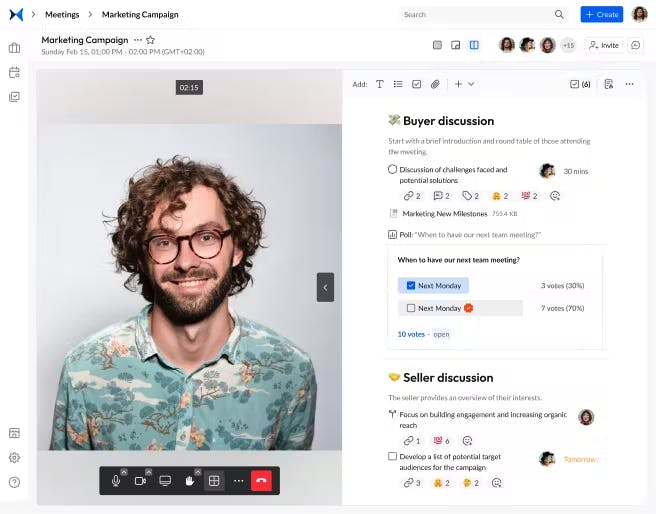
3. Comprehensive action and decision tracking to maintain meticulous oversight of patient care plans and follow-ups, ensuring no detail or update is missed in the continuum of care.
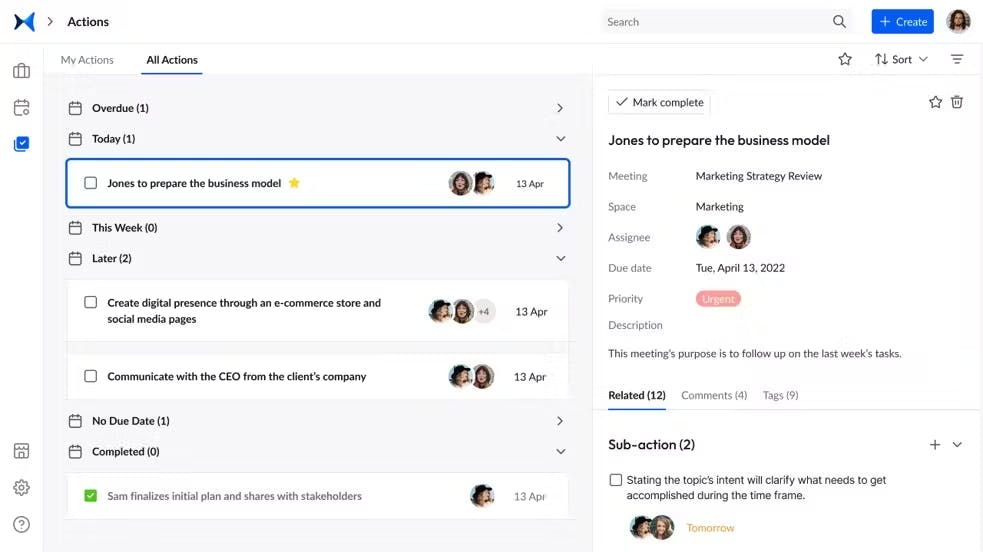
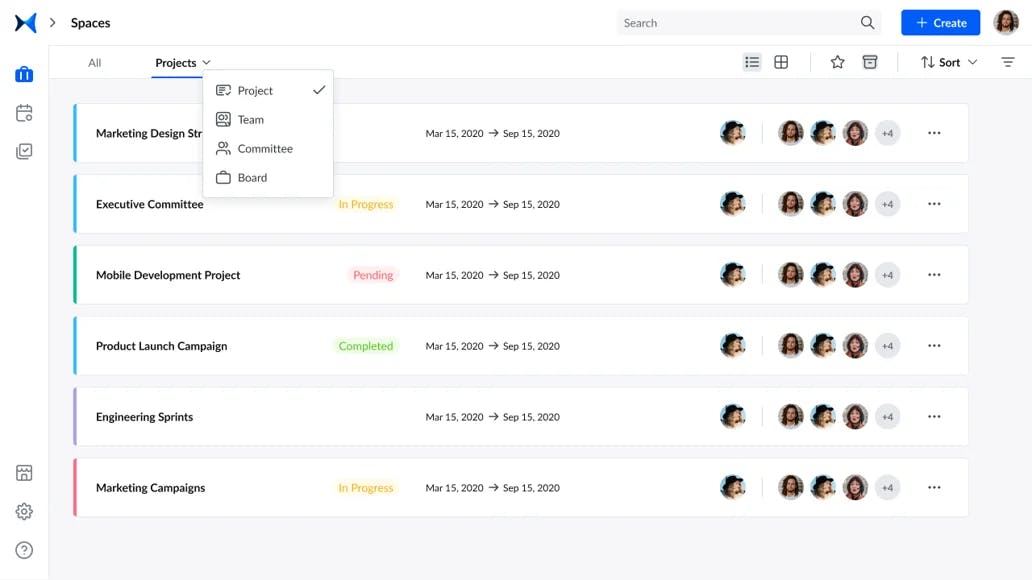
4. Organized categorization of meetings and records by teams or projects, offering a structured repository for all pertinent information on patient history and treatment plans, enhancing continuity of care.
5. Efficient generation and distribution of meeting minutes, vital for maintaining accurate records of discussions and decisions, essential for compliance, reference, and strategic planning.

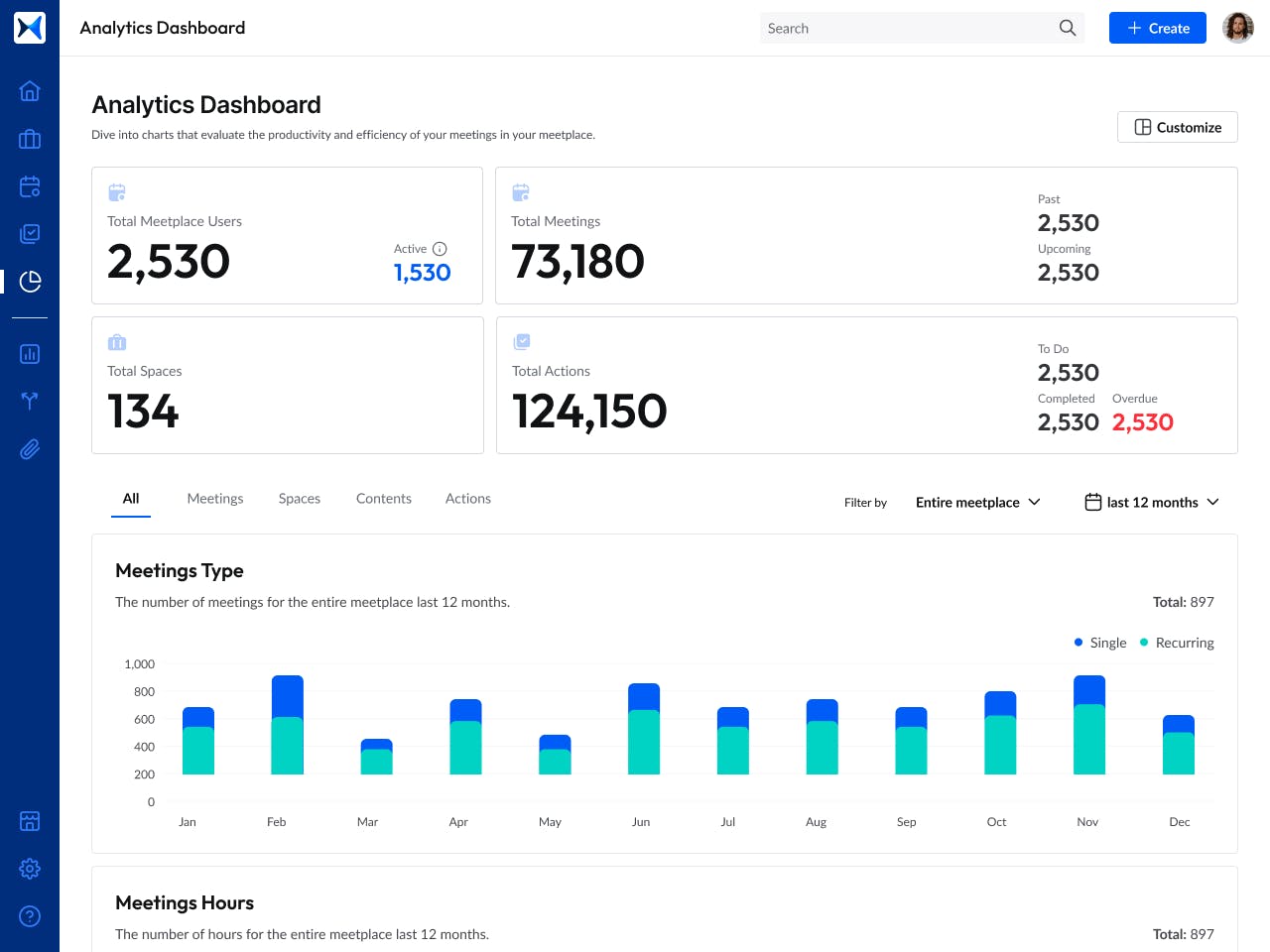
6. Access to an analytics dashboard that provides insights into participation, decision impact, and progress on action items, aiding in the continuous improvement of meeting productivity and decision-making processes.
Get started right now to streamline your telehealth and telemedicine services with adam.ai.
Transform how you conduct critical meetings—From meticulous preparation to effective execution and insightful follow-up, adam.ai integrates comprehensive analytics, full customization, and intuitive interfaces with powerful meeting management tools.
Easy onboarding. Enterprise-grade security. 24/7 dedicated support.
The bottom line
By understanding the specific applications and benefits of telehealth vs telemedicine, patients and healthcare providers can leverage digital health tools to improve care outcomes and healthcare experiences. This exploration not only clarifies their distinctions but also highlights their complementary roles in the broader context of remote healthcare services.
And while there may be multiple meeting management solutions available, here is why adam.ai is the board management software platform you can trust:
- adam.ai is one of Atlassian Ventures' portfolio companies.
- In the meeting management software category on G2, adam.ai has been ranked a leader and a high performer for successive quarters in the past years.
- adam.ai has been included in the Forrester Report in the AI-enabled meeting technology landscape.
- adam.ai is trusted and used by powerful teams and organizations worldwide for all types of critical meetings, like board, committee, project management, and business development meetings.
- And most importantly, adam.ai integrates with your existing workflow, is SOC2 compliant, provides dedicated support and success, and has a free trial option.
Subscribe to adam.ai blog
Stay ahead with the latest insights—get our newest blog posts, tips, and updates sent straight to your inbox.
